Research with Stanford Illustrates Importance of Non-Clinical Well-Being Factors
In a recent article from the New England Journal of Medicine (NEJM) Catalyst,[1] researchers from Stanford University’s Clinical Excellence Research Center and DaVita Kidney Care shared findings on how social determinants/drivers of health (SDOH) — conditions and factors outside of clinical health — play a crucial role in well-being and care management. These social risk factors include access to healthy food, stable housing, health literacy, social support, and physical and cognitive factors that can significantly influence someone’s health outcomes.
The qualitative study explored the lived experiences of people living with end stage kidney disease (ESKD) and who are dually eligible for Medicare and Medicaid insurance coverage. Interviews with nine dual-eligible patients helped researchers better understand:
- The importance of evaluating SDOH to develop effective and responsive care plans.
- The value of collaboration and care coordination across specialties including nephrology, primary care and social work to effectively identify and address SDOH in kidney care.
- The current gaps and challenges in evaluating SDOH as well as the processes and tools needed to address these challenges.
"The issue of health equity begins with the concept of dignity for each person,” Dr. Unini Odama, vice president of medical affairs at DaVita and one of the study’s authors, says. “Therefore, health equity should lead to person centered care that takes into consideration what is important to and for the person living with kidney disease. For example, what is the person’s perspective on language, social support, food and other resources they may need to ensure they have adequate opportunity to achieve their best health outcome.”
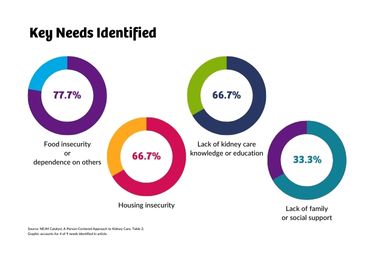
In thorough exploration of people’s lived experience managing their kidney health, researchers documented how social, functional and cognitive factors play a significant role in determining how well someone is able to manage their clinical health care needs.
“By incorporating patients’ perspectives and experiences into care planning,” Odama says, “physicians can develop more effective treatment plans. It’s not enough to provide a cookie-cutter approach, especially in kidney care.”
Holistic care, like that available through DaVita and its integrated kidney care model, provides a framework for person-centered kidney care. DaVita continues to scale these value-based programs to deliver collaborative, coordinated care across the kidney care journey, from early diagnosis through end stage kidney disease and transplantation. In these programs, patients work with an expanded care team that works together to identify and address patients’ total holistic needs with wraparound services.
The study identifies key areas where health care professionals face barriers, though. The lack of standardized screening tools and protocols specifically designed to assess social needs leaves nephrologists and caregivers without a systematic approach to identifying and addressing SDOH, for example. Additionally, nephrologists often face limited time during consultations, making it difficult to uncover social drivers and address them adequately.
“Despite these challenges, nephrologists are increasingly recognizing the significance of SDOH and are motivated to find solutions,” Odama, says.
Odama is helping to lead and support key initiatives at DaVita that aim to address SDOH as part of its Strategic Kidney Health Equity Framework.
In addition to comprehensive integrated care programs, DaVita is working internally and with others to address challenges patients may face.
Through DaVita’s work with the American Diabetes Association (ADA), they are looking to increase kidney health awareness for people living with diabetes and, as a result, living with a higher risk of kidney disease. The DaVita Giving Foundation also announced a grant for the Food Is Medicine Coalition (FIMC), which provides access to medically tailored nutrition for people who are facing the dual crisis of food insecurity and chronic illness. In 2023, the grant helped provide more than 160,000 meals to eligible individuals.
As the organization continues their mission to improve equitable care, the study with Stanford University has reinforced the need to look at individual needs.
“Providing person-centered care requires that we move past treatment alone, to treatment plus caring about social factors that influence kidney health care,” Odama says. “Furthermore, our caring skills sharpened by empathy will enable us continue to deliver more person centric and equitable care to persons living with kidney disease.”
Please visit NEJM Catalyst for more information on the study, A Person-Centered Approach to Kidney Care.
[1] Victoria Liou-Johnson, PhD, MS, Aditya Narayan, Unini Odama, MD, MPH, MBE, Katy Weber, MPH, and Nirav R. Shah, MD, MPH; “A Person-Centered Approach to Kidney Care;’ New England Journal of Medicine Catalyst; https://catalyst.nejm.org/doi/full/10.1056/CAT.23.0376








